“…it does appear as though the virus is evolving in that direction—and more quickly than would be expected naturally, thanks to antiretroviral therapies.” motherboard
Tag Archives: infection
the eric update – day 55: please keep your seatbelt tight and your hands safely inside the car.
today was quite exhausting, but in the end it might hopefully be best remembered as eric’s first, big false alarm. he started “alarming” ( meaning his breathing stopped and his heartrate would drop to dangerously low levels ) suddenly over the prior night and he kept it up through the morning. protein showed up in his urine which normally might not cause immediate concern. but it could possibly indicate a blood infection; taken with the increase in alarms, and his previous history of “crashing” fast, the staff went into “red alert” mode and started running tests to try to narrow down what was going happening. ( in this photo, eric is remaining remarkably calm, despite having a bag taped to his groin to collect urine for a more extensive analysis. )
coincidentally, eric’s neonatal nurse practitioner was also on duty during his prior two “crashes” and made it clear that she was being hyper-vigilent. in a sense, it was reassuring to know that someone was watching his every move who was intimately aware of his ability to crash suddenly and without many of the normal warning signs ( trouble digesting food or bad blood gasses or immune cell counts ). she talked with us for quite some time about how strong a fighter he was, but that it can be more difficult to know how to treat him; unlike a “wimpy white boy” who will wear his ailments on his sleeve, he fights and fights and fights and looks fine, until he can’t fight anymore and crashes fast.
when we talked in the morning, the n.p.p becky was leaning towards the theory that eric was suffering from a bug that wasn’t responding completely to his antibiotic treatments. looking over his record, she thought she could see a pattern of getting sick 4 or 5 days after being taken off antibiotics. by noon she was so convinced of her theory that was prepared to start him on “big boy” antibiotics ( the nurses term for antibiotics which are reserved for treating the nastiest of the nasty bugs ) even without any strong evidence that he had an infection.
in the end, after hours of alarms and lots of theories about what may or may not be happening, they decided to turn up the rate of air flow on his nasal cannula and he stopped all of his “naughtiness” ( nurses term for when babies alarm ). it’s impossible to describe what it’s like to spend the day trying to muster the energy to yet again prepare for the worst, only to things quiet down after fiddling with knobs.
a false alarm? we’ll know more if he makes it through the night without any more problems.
after the staff turned up his flow, he start to get less listless and more active ( a good sign, since turning into the equivalent is one of the possible signs of an impending infection ).
as we prepare to leave for the evening, eric decides that he’s ready to bust out of the nicu and attempts to wiggle off the radiant warming bed.
the eric update – day 44: almost closed pda. bugs? and more bugs?
i think eric is enjoying dragging out the drama of doubling his birthweight. he was up 10 grams today, topping the scales at 1270 grams or 2 pounds 12.8 ounces.
we finally received word on his patent ductus arteriosis and it’s almost amusing – it’s not closed, but it’s not open wide enough to warrant additional measures to try to close it. although everyone seemed quite confident that it would close on its own, it’s still slightly disconcerting to not be able to give a definitive answer to the innumerable questions regarding the status of the hole in his heart. i didn’t follow up as rigorously as i might normally as to why they weren’t going to pursue another round off indomethacin simply because everyone seemed so confident that the hole wasn’t big enough to have any physiological consequences and that it would close on its own accord.
unfortunately, i don’t have any good an answers as to what may or may not be the source of his sepsis ( if, in fact, he does have a blood infection ). remember, they caught a gram negative bug in a blood sample that was being used to determine if he had a yeast infection. they’ve been having trouble determining the exact type of bug in the sample because, as a person from “infectious diseases” said today – “fungus is funky”. in other words, they are trying to grow enough of the bacteria to allow identification in a media that was meant to grow fungus and it’s not working well. all you armchair microbiologists in the crowd could perhaps speculate as to why they can’t transfer the small amount of the bacteria they did find into a more suitable media. then again, i might have some of the details confused so it might not be worth your effort. luckily they haven’t found any bugs growing in any other samples they’ve drawn, so all this might be much ado about nothing.
we also received the results from another round of “trach aspirate” tests, which indicate if he has anything growing in his trachea ( being intubated on the vent greatly increases the chances that strange bugs will grow in his trachea ). six days ago, they discovered small amounts of enterobacter and klebsiella growing in his trachea and today they said the bugs were still there, despite being on antibiotics for nine days. the staff seem to not be overly concerned about the bugs sticking around for now. things might be different if they are still there after they finish the antibiotic regime, which will last for about 6 six more days.
oh. and his arm was quite red around the entry point of his IV line, which would strongly indicate that a superficial bacterial infection was starting. they moved the line and applied a topical antibiotic which will hopefully prevent any further complications.
i was joking with the nurses that i didn’t have any of these problems with bugs when i was a 26 weeker, 32 years ago, and that one couldn’t help wonder whether or not eric IV had the misfortune of finding himself in a “dirty” unit ( really, it was all in good humor ). aside from being continually astounded that i survived the ordeals of being a micropreemie in 1972 ( indeed, one nurse commented that when she started in the nicu at about that time, they would have never tried to save a 28 weeker, little less a 26 weeker ), the nurses all remind me that we can thank indiscriminate usage of antibiotics for causing all the “bug” problems that are seen in the modern nicu.
so think about the micropreemies the next time you jump for the medicine cabinet to grab an antibiotic for a minor ear infection.
the eric update – day 39: improving. or not, depending on your perspective. and poundcake!
in the new world that kris and i live in, the world where things can go from good to horribly bad in three hours and we’re constantly trying to come up with new and innovative strategies to prevent us from turning into the weak-willed people with the small brains who run shrieking into the burning wreckage, it still would have been impossible to predict ahead of time exactly how we’d react to a 6 a.m. nicu phone call that resulted in us discovering that eric had been diagnosed with pneumonia, mere six hours after being told that his clinical picture was improving.
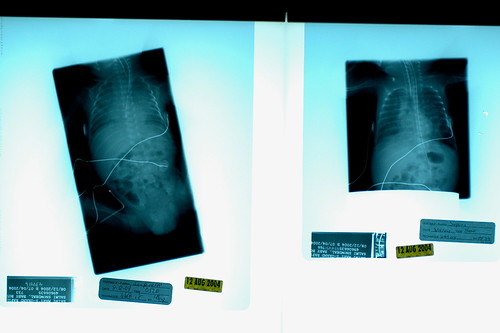
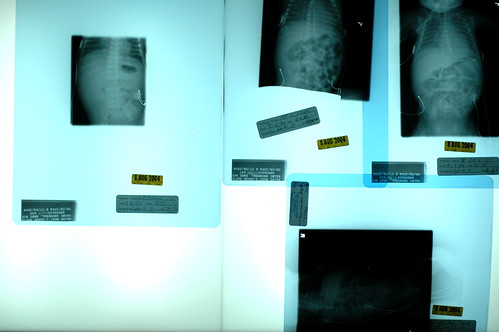
instead of shrieking, we found ourselves confusedly attempting to discern the implications of the cruel laws that we apparently must learn to abide by in our new world. “but you said he was improving?” kris queried. “oh, he is!” the caller stated, perhaps a bit too emphatically. i pondered what we should prepare ourselves for if he really starts improving. slowly, we discovered that, occasionally, the progression of pneumonia is such that you really can start improving before you ever get diagnosed as having the condition. in other words, the classic hazy x-rays which conclusively indicate pneumonia can appear after you’ve already started to gain ground on the bugs that cause the effect. so he was improving, in terms of his blood count differentials and other immunse system indicators, but our mistake was in believing that by using the word “improving” the staff really meant that eric had escaped getting another diagnosis put on his permanent record. apparently we were wrong.
getting the pneumonia diagnosis is quite normal for a micropreemie, as nurse donna’s unscientific estimate was that 90% of babies born prior to 28 weeks get the condition ( incidentally, i suspect that a micropreemie parent can’t not begin to hate to hear the various trials and tribulations that their child must suffer through described as “normal”. ), and 50% of children born so soon will develop pneumonia more than once during their stays at the nicu. since eric’s lung x-rays indicate that his lungs are already beginning to recover, i suppose we need to focus on the fact that things could have been much, much worse. even so, barring any complications, eric probably won’t fully recover from pneumonia for 2-3 weeks. while he likely won’t need to be on the vent for the entire time, we’ve noticed that the staff has stopped making predictions as to when he’ll be off the vent.
it’s hard to imagine what tomorrow will bring.
oh. and in an attempt to accentuate the positive, i should note that eric weighed in at 1075 grams or almost 2 pounds 6 ounces.
update: in my tiredness when i posted this last night, i forgot to mention the highlight of our day – the arrival of two pounds of rowena’s pound cake with “curd” sauce that my sister candy sent to celebrate eric hitting the two pound mark! it was a very sweet gesture. literally 🙂
candy mailed the pound cake to my home ( she’s family, so she gets to do that ) and i cleverly took it to the nicu right before the shift change, so that both the day and night shifts could enjoy the gift ( bonus points for me! ). i can say without a doubt that everyone enjoyed the cake.
the eric update – day 38: improving. but bugs and decreased lung function looming.
the good news is that eric’s overall clinical picture is improving, even though he is still on the vent, which is to say that his blood counts are showing that his systemic infection is nearly gone and his blood gas profile is looking great. the shortest answer as to why he’s on the vent for longer than he’s ever been is that they are concerned that they want to make sure that his bowels are completely recovered after shutting down the other day before they put him back on cpap. the armchair reseachers in the crowd can investigate why cpap is bad after an illeus ( the technical term for the lower bowels stopping to function ) because i haven’t had the time to put all the pieces together.
although his overall status is improving, we were warned about a few new issues that are developing. after 5 weeks of not needing much supplemental oxygen, eric is starting to need to have his ‘ooooooh’ increased; in other words, while he’s done remarkably well in the past breathing unenriched room air ( with around 20-21% oxygen) , he’s now consistently needing 25-40 percent oxygen in his air supply. of course, there are several reasons why he might be needing more oxygen.
most innocuously, he might simply be getting comfortable on the vent and getting lazy, taking fewer and shallower breaths. breathing takes a lot of work, and if the machine is going to do the heavy lifting, many micropreemies are more than happy to take a breather from breathing and require a little more oxygen to keep their blood gas levels at appropriate levels. while this might be partly the cause, he respiratory profile doesn’t indicate that he’s getting too lazy, so my guess is that it’s only playing a minor role.
slightly more disconcertingly, he may also be developing a tracheal infection, which can irritate his mucous membranes and produce more slime and goo than normal; more slime and goo makes it more difficult to breath and increase the need for supplemental oxygen. he certainly seems to have more secretions than normal of late. and indeed, while we were discussing the potential for trach bugs, eric’s latest labs came back and he was positive for enterobacter and klebsiella which are gram negative nosocomial bugs – in other words he got an infection from bugs that you find in the hospital. while it’s not something that you want to see, it would be more remarkable if he didn’t get a nosocomial infection from all the tubes entering various parts of his body. technically, the bugs have simply colonized and have not shown any evidence of becoming particularly invasive. simply put, they are just hanging out and slowly multiplying around his ET tube and don’t seem too concerned with overtaking his system. it’s very difficult to pummel colonized nosocomial bugs into complete submission so they are going to wait and see if eric’s nascent immune system can keep them in check. i guess you could call this a developing story that could “get legs” and hit the front page soon.
perhaps even more problematic is the fact that eric could be developing a lung condition known as chronic pulmonary insufficiency of prematurity (cpip). essentially, this means his lungs are not growing fast enough to keep up with the oxygen requirements demanded by his growing body. cpip presents itself similar to bronchopulmonary dysplasia (bpd), but they are actually different enough to warrant different treatment strategies. this evening nurse practitioner dawn was not willing to say that he definately had cpip, but she said it wouldn’t surprise her at all to see him get the official diagnosis over the coming weeks. the good news is that if he does have cpip, he will quite likely eventually regain normal lung function ( perhaps by year 2 ). the not-so-good news is that cpip could necessitate that he leave the nicu with an oxygen tank.
just in case you’ve started to miss the forest for the trees, the good news is that eric’s overall clinical picture is improving.
and we’re still getting postcards ( scroll down to the bottom of the link )!
the eric update – day 35: i want off this ride.
three hours. that’s how quickly things can go to hell in a handbasket. we left at 11 p.m. last night, as confident as ever that we had escaped any problems which seemed to be lurking in the background all week long; by 2 a.m. several of eric’s systems were failing all at once and by 4 a.m. there was serious concern that he might have a perforated bowel and they were getting ready to transport him to the other nicu in town for emergency surgery. at the time, apparently the only thing that kept eric from being transported was the fact that the surgeons said that they wouldn’t do the surgery on him because he was too small to survive.
the following twelve hours were filled with as many, if not more, emotional ups-and-downs than the night eric was born. as the complications were delineated it became apparent that he had not one, not two but three calamitous events occurring, two of which were characterized as rare. the most acutely dangerous event was known as a strangulated hernia ( ironically, the determination that he did, in fact, have a hernia was considered so uneventful that i decided not to post such boring news right away ), which happens when fecal matter gets pushed into the herniated bowel and can quickly lead to a perforation. and the last thing you want with a micropreemie is a hole in the intestine, leaking fecal matter and air throughout the abdomen. it’s quite uncommon to see a strangled hernia in a micropreemie; only one of the nurses could remember an occurrence, 7 years ago, and couldn’t remember having seen any prior incidences. somehow the neonatologist was able to unstrangulate his hernia by holding him upside down and pushing and poking at the hernia. in a very understated way, the neonatologist would later allude to just how lucky we were that her improvised unstrangulation technique worked, as i’m not sure what would have been done since it was already determined that they weren’t going to perform surgery on him on account of him smallness.
why was fecal matter being so forcefully pushed through his hernia? because it didn’t have any place to go as his bowels were shutting down and everything was stopped from moving along normally. in addition to creating a strangulated hernia, his backed up bowels quickly began pushing on his lungs, which stopped his breathing and necessitated eric being put back on the vent. and why were his bowels shutting down? a quick blood panel indicated that he was quickly getting an infection ( as evidenced by an increase in immature neutrophil cells or bands ), and his body began shunting blood away from his bowels and towards other areas in preparation for a battle royal. routing blood away from the intestines is likely a good strategy most of the time, as who has time for eating when you’ve got a bad infection, right? unfortunately when you’ve got 7 cc’s an hour of breastmilk coming in and blood moving out, you’re actually creating the best possible conditions for necrotizing enterocolitis.
as if a strangulated hernia, backed up bowels and a worsening general infection weren’t enough to make for an exciting night, the nurses discovered that while they were trying to unstrangulate his hernia, his skin was sloughing off. yes, you read that word right, his skin was falling away. disintergrating. and creating a festering mess. for a little thought experiment, try to imagine having to absorb the word sloughing at 4 in the morning. at the time the disintegrating skin was perhaps the scariest news, because nobody had seen anything like it. nobody. in the morning nurse jan confessed that she hadn’t seen it in 22 years of working in the nicu. even the infectious disease specialist hadn’t seen anything like it.
oh, how we were wishing for good old days, when the worst we had to worry about was whether or not he’d be put back on the vent.
so the day was spent trying to come to grips with how quickly and how completely everything had fallen apart, as we tried to stay focused on how his clinical pictures was changing from moment to moment. an antibiotic regime was started to help fight the general infection and they decided to treat the mystery topical infection with pretty much everything they had as they were lacking any any definitive specific lab results ( no trace of yeast in the infection and no bugs are caught growing; the lack of any yeast was described and bizarre, since you’d expect to see some and as we learned in the past, it’s not that surprising to not catch the bugs ), they decide to treat it as if could be anything, which i guess is just about the only thing you can do. as the day wore on, his blood counts began to slowly return to normal and by the evening almost all evidence of the skin sloughing had disappeared.
it’s hard to describe the feeling that you’re left with as you realize that the wreckers of such rare havoc are going to fade away without you ever knowing their names.
it took quite some time for the neonatologist to rule out a bowel performation, as the regular x-rays kept showing large amounts of air in his bowels and it was difficult to know if the air was inside or outside the intestine; a specialized x-ray machine was hauled in which could more easily allow them to determine if the air was moving as he changed positions, which would mean that it was floating around his abdominal cavity.
as luck would have it while the film was being processed, there were two more admits to the nicu, which meant that we had to sit around, wondering when they’d get a free second to review the results and release us from the purgatory of not knowing if he had a perforation. eventually, the neonatologist rushed in and exclaimed that everything looked great and that we were out of immediate danger for now.
it’s funny how quickly you can reset your personal expectations as to what constitutes good news. before we left for the night we watched eric resting comfortably on the vent, feeling a sense of relief to see him so peaceful while pondering the irony that today’s good news would have been yesterday’s catastrophe.
many, many thanks to all of eric’s wonderful caregivers whose attentive observations and quick, accurate actions helped to avert what surely could have been a disaster. i’ve said it many times already, but i have no idea how you do what you do.
the eric update – day 13: a mostly lazy day
today was a very boring day with not a single, solitary alarm; well maybe this is not quite true actually, as the nurses will typically induce apnea during some of their procedures, but nobody counts those. except maybe for eric.
he’s still on the vent, but they are continuing to gradually reduce the settings and suspect that perhaps over the next few days he might be able to go back to the less abusive CPAP regime. this is surprisingly good news, because the staff has been suggesting for the past few days that he could possibly be on the vent for a couple of weeks.
and his infection seems to be getting better. there’s still no definitive results to indicate what sort of infection he might have, but all of his differential blood counts are looking more positive and his blood sugar is normalizing.
during a quiet moment, i catch kris holding eric’s hand/arm. he just had a few procedures done that he didn’t care for and she’s using a technique that the nicu staff taught us to calm him down – i.e. he feels more secure when you firmly hold his arms and legs against his body. it gives him a sense of boundary that he got used to in the womb.
so, with a lack of white-knuckle events to pass the time, we found ourselves enjoying just sitting around his bed, reading more from winnie-the-pooh, talking with the always informative and mostly cheery nicu staff and just generally having what passes for a lazy saturday these days.
it’s amazing how much his skin changes from day to day, depending on whether or not he’s received a transfusion or how much fluid he’s retaining.
today he seems particularly wrinkled.
every so often he’d open his eyes and watch me taking pictures, but he didn’t seem to want to keep them open for long.