woohoo! we received a phone call from the nicu to not be freaked out when we arrived and found an empty radiant warming bed, since eric had been moved to an isolette! it’s a big step up, as the isolette is the step before an open, unheated bed, which is the step before going home.
after the move to the isolette, they removed eric’s temperature sensor that constantly monitored his body temp. this means that they are increasingly confident in his ability to regulate his own body temperature, which is one of the “exit criteria” for leaving the nicu. the isolette is still heated to keep a thermoneutral environment, which is the temperature that is needed to prevent him from burning any calories on keeping warm, as they’d like every bit of evergy to go towards growing and staying healthy. that said, they will slowly ween his off the thermoneutral settings, at which point he’ll get transferred to an open bed.

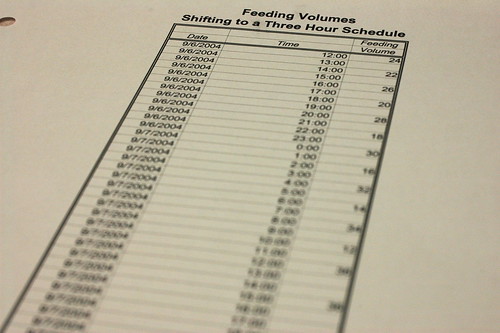
eric also took his first bottle today! i think it might be impossible to convey to non-nicu parents what a big step it was for him to guzzle down a bottle on the first try. it can sometimes take weeks for a micropreemie to get the suck-swallow-breath sequence down for an entire 20 cc bottle.

nurse nancy got the process started because she wanted to make sure he didn’t drown, but he did so well that she quickly transferred him over to kris so she could enjoy the moment.

gulp. gulp. even more amazingly – nurse nancy used a newborn nipple and not a preemie nipple, which makes it that much more difficult to get the milk. that means he’s got a pretty strong suck reflex.

maybe he’s looking for a “high five”?

it’s time for a burb. as always, things are more complicated with a micropreemie, so it takes a bit to figure out how to burp him without accidentally stopping his breathing.

nurse nancy shows kris how to stimulate eric’s suck reflex.

who knew feeding could take so much effort. after the bottle is finished, eric falls fast asleep.

kris watches his monitor after the feeding. all the food in his belly can stimulate his vagus nerve which affects his heartrate and can lead to a “brady” ( bradycardia – a dangerous slowing of his heartreate ).
after nurse nancy saw how well eric was doing with the bottle, she casually asked us how the nursery looked. we looked at her blankly.
“uh. the nursery is still an office.”
she looked shocked and then said something that neither one of us could possibly have expected. “well, what are you going to do if everything “clicks” and he’s released in two weeks! get your butts in gear! have you taken the infant cpr class? have you watched the “shaken baby syndrome” video? there’s lots to do and he’ll be leaving quite literally before you know it.”
kris responded with exactly what i was thinking as my mouth went dry, “nancy. your lips are moving but there’s no sound coming out.”
before today i had been trying to manage my expectations and thought that if we were lucky, eric might be home by the last week of october or the first week of november. this hadn’t seemed an unreasonably assumption since the the neonatologist told us when we arrived that eric would most likely be in the nicu until his original due date ( around actober 17th ) plus ” a few weeks”. so it’s no small shock to find out that it’s not outside the realm of possibility that he could be home soon. she did say that it probably wouldn’t be exactly two weeks, but my guess is that they are likely looking at 2 weeks to a month. it’s odd to think that if he were released even in a month, he’d be coming home a full three weeks before his original due date.
i guess it’s time to get cracking at turning the home office into a nursery.

even though the isolette is considered a big move, is still takes a bit of adjustment to get used to the new environment. after two months of having unobstructed access to eric, it’s hard to get used to having to reach into a “box” to say “goodnight”.
there’s also a lot less space around the isolette, since it’s less likely that a large number of personnel will need to gather around eric for an emergency intervention. and we’ve moved from a a quiet, corner on the far end of the room ( the room is a rectangle with the sickest babies at the far end of the rectangle and the healthiest babies at the near end close to the entrance ) to right next to the nurses station and the entry door, so it’s a lot more noisy.
i guess any change, no matter how positive, takes some adjustment.