eric was “throwing” more alarms than usual today. mostly apnea ( forgetting to breath ) and bradycardia ( slowing of the heart rate ). while completely normal, it can still get tiring to sit, staring at the monitor, with a hand ready to rub his back or the bottom of his foot to jumpstart his breathing, if the alarms start. last evening he had 6 apnea/bradycardia incidents alone and he had 8 more over the night. typically, he might have 3 or 4 in an entire day – so the rate has definately increased.
when micropreems are having trouble breathing it means, at best, that they are getting tired and at worst something else is going on, such a systemic infection ( in this particular case, it’s probably not a generalized infection, since they didn’t see an elevated white blood count in his latest labs ). in either case, you’ll often see a range of systems start to work less efficiently as things start to slow down. and when that happens, the nicu nurses have to do many unpleasant things to your baby while you watch. this is the sad part of their job and they are all the more heroic for doing it day in and day out.
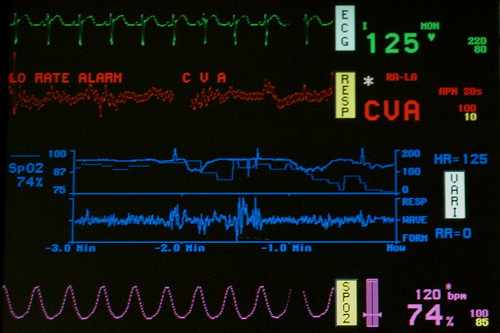
the machine creates a quick succession of “bing! bing! bing!”, if his pulse/oxygen levels dip along with his heartrate creating a “low rate alarm”. this is not necessarily a concern, but rather a warning.
a different and more urgent sounding pattern of “bings!” emanates from the machine if the “low rate warning” progresses to full-blown apnea ( not breathing ). at that point nurses will start running to the bed, while you try to remain calm.
eventually, when they see that you’re not going to turn into a mass of useless flesh when the alarms start ringing they’ll teach you how to see that your son really isn’t breathing ( i.e. it’s not a false alarm ), and they’ll show you a variety of ways of getting him “jumpstarted”, ranging from rubbing his back in a specific spot to tapping his butt or the bottom of his foot.
today i got him breathing a handful of times over a few hours, which i guess constitutes a form of bonding. right when i snapped this picture he went into full-blown apnea and i had to drop the camera and rub his back, so i could only get a shot of the less urgent “low rate alarm”.
the nurses are going to put him back on CPAP full time, since the nasal cannula takes a little more work on his part and if they need to start “bagging him” ( ventilating him manually with a small bag like you might see on the tv program ‘ER’ ), then it’s possible that they might put him back on the oscillating vent. i don’t even think they’d call it a set back, but rather he’s just telling us that he’s tired and would like us to take over for awhile while he recoups.
another sign that he’s getting tired came when they suctioned the contents of his stomach and found 1.5 cc’s of undigested colestrum. they are giving him 0.5 cc of colestrum every 2 hours, so clearly his digestion has slowed. if the food sticks around for too long then a condition known as necrotizing enterocolitis (NEC) – which are a big couple of words for rotting bowels – can set in quickly, as the blood supply to his bowels is decreased or interrupted. under those conditions, hypoxia ( lack of oxygen in the tissue) can kill or damage the cells in the bowel wall, eventually leading to perforation and peritonitis ( infection of the abdominal cavity ). advanced NEC is something you don’t ever want to see, since it requires very difficult bowel surgery, so they’ll be watching him closely.
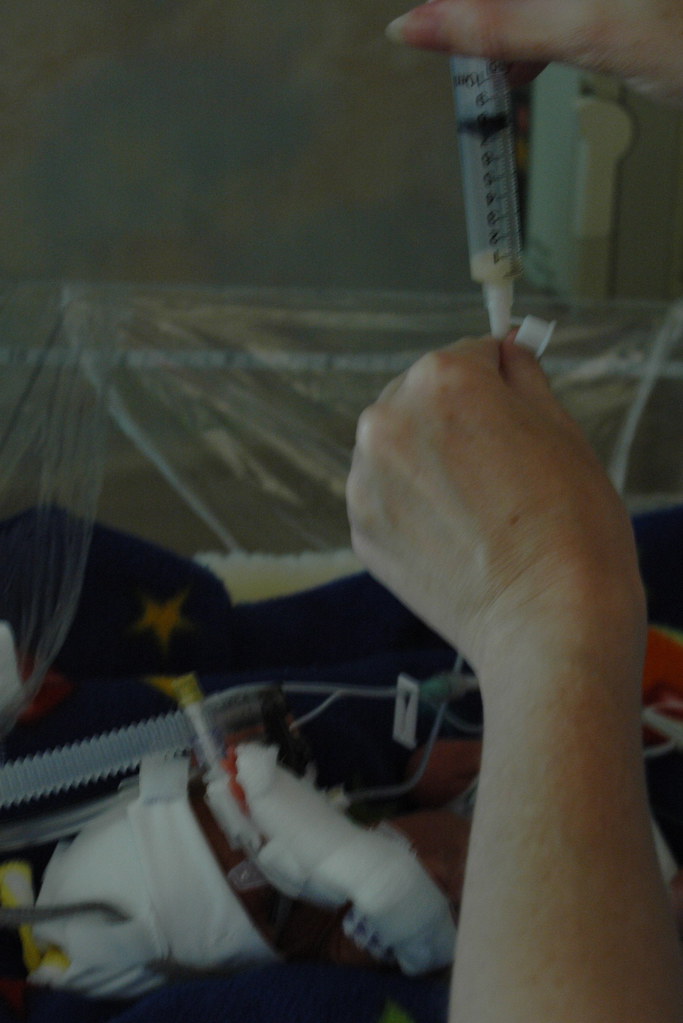
in this picture, eric is suffering through the least of his abuses as nurse peggy is pulling the undigested contents of stomach out through his endo-tracheal tube. he gets a half a cc at each feeding and she pulls out 1.5 cc’s, so he’s not digesting much.
right before nurse peggy sucked out the contents of his stomach, she aspirated his nasal passages to increase air flow. it sounds innocuous enough, but it involves threading about six inches of tubing through his nose, into his sinuses and down his throat, all the while rotating and thrusting the tube to suck out any last drops of mucus.
after hours and hours of alarming and being probed and prodded and “jumpstarted” the alarms have settled down and he’s looking like he might be stabilizing.
he eyes us warily as nurse peggy tells me that he’s doing well, all things considered.
so, in the end, today was quite demanding and typical of the rollercoaster that a 24 weeker can put you on; and when juxtaposed against what happened yesterday, today was a great reminder that one needs to focus on enjoying each moment for what it is.